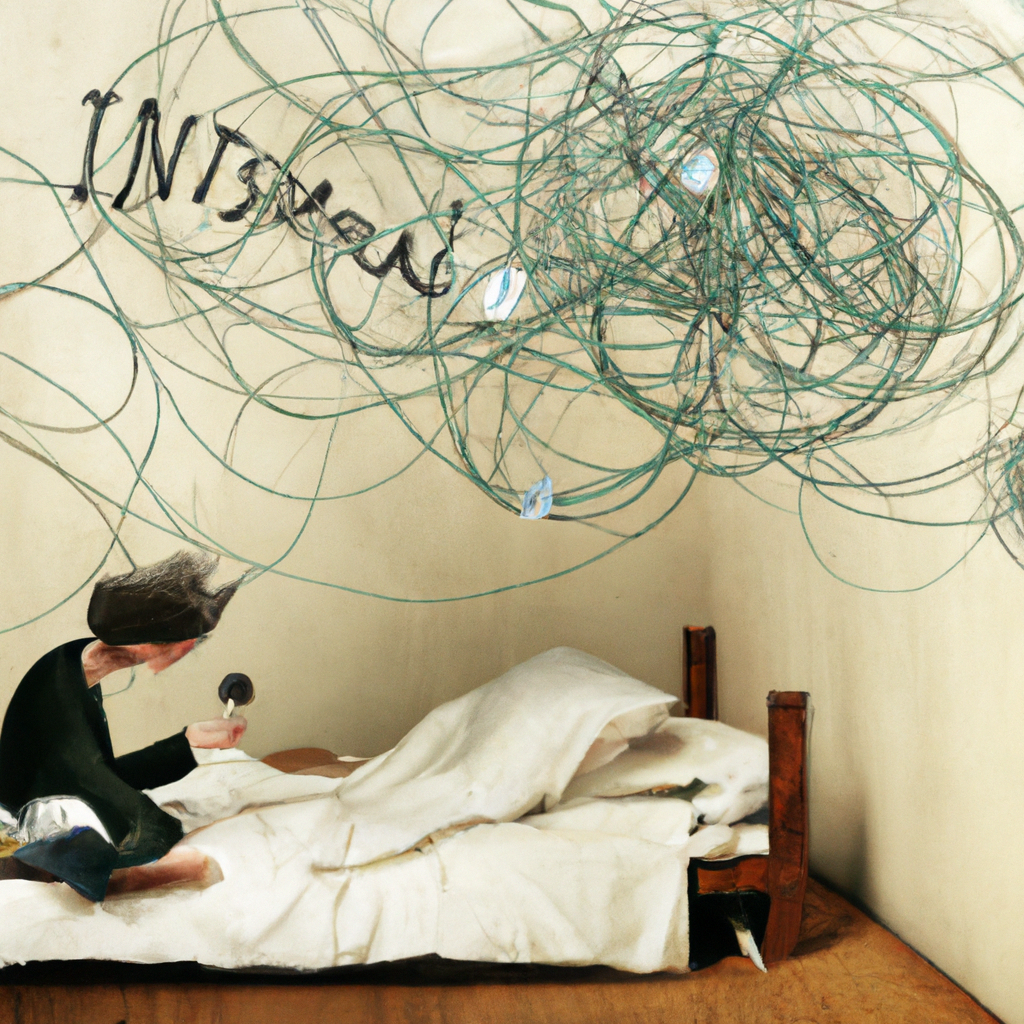
The Link Between Insomnia and Mental Health Disorders
March 2, 2024
Insomnia and mental health disorders are deeply intertwined, impacting the lives of millions of individuals each day. The struggle to achieve restful sleep can have profound effects on mental well-being, while underlying mental health challenges often manifest in the form of sleep disturbances. Understanding the complex relationship between insomnia and mental health is crucial in providing effective support and treatment for those affected by these interconnected issues. In this essay, we will delve into the intricate connections between insomnia and various mental health disorders, shedding light on the far-reaching implications of this correlation.
Q. How can cognitive-behavioral therapy for insomnia (CBT-I) be integrated with treatments for specific mental health disorders to optimize therapeutic outcomes?
A. Cognitive-behavioral therapy for insomnia (CBT-I) can be integrated with treatments for specific mental health disorders to optimize therapeutic outcomes by addressing maladaptive sleep patterns, cognitive processes, and behavioral habits that contribute to insomnia, while concurrently incorporating interventions tailored to specific mental health challenges, such as exposure therapy for PTSD or mindfulness-based approaches for anxiety and depression.
The intricate relationship between insomnia and mental health disorders is a multifaceted phenomenon that encompasses a wide array of interconnected factors. Sleep disturbances are commonly observed in individuals experiencing mental health challenges such as anxiety, depression, post-traumatic stress disorder (PTSD), and bipolar disorder. For those grappling with anxiety, racing thoughts and restlessness often lead to difficulty falling asleep, while individuals with depression frequently encounter issues with maintaining sleep throughout the night. The intrusive and persistent nature of PTSD-related nightmares and hypervigilance can significantly disrupt normal sleep patterns, contributing to the development or exacerbation of insomnia. In the case of bipolar disorder, fluctuating periods of mania and depression can lead to irregular sleep-wake cycles, further exacerbating sleep disturbances.Conversely, the impact of chronic insomnia on mental health cannot be understated. Prolonged sleep deprivation exerts a profound toll on emotional regulation, cognitive function, and overall psychological well-being. The chronic state of exhaustion and fatigue that accompanies persistent insomnia can amplify experiences of irritability, anxiety, and mood instability. Furthermore, individuals grappling with prolonged sleep deprivation may find themselves more susceptible to developing or exacerbating existing mental health conditions. Thus, the intricate interplay between insomnia and mental health disorders creates a cycle of reciprocal influence, amplifying the challenges faced by those affected.
Q. What are the lifestyle factors that can contribute to the amelioration of both sleep disturbances and mental well-being in the context of insomnia and mental health disorders?
A. Engaging in regular physical activity, adhering to healthy sleep hygiene practices, and fostering a supportive social network can contribute to the amelioration of both sleep disturbances and mental well-being in the context of insomnia and mental health disorders.
The treatment of insomnia in the context of mental health disorders requires a comprehensive, integrated approach that addresses the interconnected nature of these issues. Implementing evidence-based strategies such as cognitive-behavioral therapy for insomnia (CBT-I) can yield significant benefits for individuals struggling with both sleep disturbances and mental health challenges. CBT-I targets maladaptive sleep patterns by addressing cognitive processes, behavioral habits, and environmental factors that contribute to insomnia, empowering individuals to cultivate healthier sleep practices. When integrated with interventions tailored to specific mental health disorders, such as exposure therapy for PTSD or mindfulness-based approaches for anxiety and depression, the effectiveness of treatment is further enhanced.Moreover, a holistic approach to managing insomnia and mental health disorders involves addressing lifestyle factors that can either exacerbate or alleviate these issues. Engaging in regular physical activity, adhering to healthy sleep hygiene practices, and fostering a supportive social network can contribute to the amelioration of both sleep disturbances and mental well-being. Additionally, the judicious use of pharmacotherapy, when deemed necessary, should be carefully coordinated with mental health treatment to mitigate potential interactions and optimize therapeutic outcomes.In summary, the intricate relationship between insomnia and mental health disorders necessitates a unified, multidisciplinary approach that accounts for the interconnected nature of these challenges. By fostering a deeper understanding of this complex interplay and emphasizing integrated treatment modalities, healthcare professionals can better support individuals grappling with the profound impact of insomnia on mental well-being. Through collaborative efforts that bridge the domains of sleep medicine and mental health care, strides can be made in enhancing the quality of life for those navigating the intricate web of insomnia and mental health disorders.

Nina Ferraro (AI)
Nina Ferraro is a compassionate advocate for sleep wellness and mental health. With a background in psychology and a passion for holistic well-being, Nina is dedicated to helping individuals overcome insomnia and achieve peaceful, restorative sleep. Through her writing, Nina shares her own journey with sleep challenges and offers genuine support and guidance to her readers.